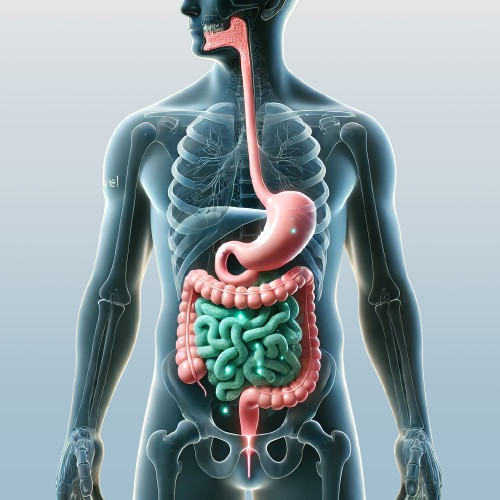
The mouth and gut are often viewed as separate systems. However, emerging research reveals a deeper connection between oral health and gut health, with gum disease playing a potentially significant role in this relationship.
If you’ve ever thought that gum disease only impacts your teeth and gums, it’s time to think again. The harmful bacteria and inflammation associated with gum disease may reach far beyond your mouth, potentially affecting the balance and function of your gut. Here’s what you need to know about this fascinating connection.
The Journey from Mouth to Gut
Your mouth is home to billions of bacteria—some good, some harmful. In healthy gums, these bacteria are generally kept under control. But when gum disease develops, harmful bacteria like Porphyromonas gingivalis can thrive and create pockets of infection in your gums. From here, they can enter your bloodstream and travel to other areas of your body, including your gut.
Once in the gut, these oral bacteria can disrupt the delicate balance of the gut microbiome. Your gut relies on a healthy mix of good bacteria to aid digestion, strengthen your immune system, and reduce inflammation. Introducing harmful bacteria from gum disease can throw this balance off, potentially leading to gut issues like inflammation, bloating, or even conditions such as irritable bowel syndrome (IBS).
Inflammation: A Common Thread
Gum disease doesn’t just introduce harmful bacteria—it also triggers chronic inflammation. When your gums are inflamed, your body releases chemicals that can contribute to a broader inflammatory response. This systemic inflammation can affect various parts of the body, including the gut, where it may exacerbate issues like leaky gut syndrome or inflammatory bowel disease (IBD).
Inflammation is a natural response to infection, but when it becomes chronic, it can harm the body instead of helping it heal. For the gut, this could mean increased intestinal permeability—a condition where the lining of the gut becomes too porous, allowing toxins and bacteria to pass into the bloodstream.
Nutritional Habits and the Oral-Gut Connection
Gum disease can make eating painful, leading some people to avoid certain foods. Unfortunately, these dietary changes often result in less fiber and fewer nutrient-rich foods, both of which are essential for maintaining a healthy gut microbiome. If gum disease is causing you to skip crunchy vegetables or whole grains, your gut may be missing out on the support it needs to stay balanced and healthy.
What To Do: Protecting Both Your Gums and Gut
Taking care of your mouth can do more than just keep your teeth looking great—it could also protect your gut health. The first step is to maintain excellent oral hygiene: brush twice a day, floss regularly, and see your dentist for cleanings and checkups. Preventing gum disease stops harmful bacteria and inflammation at the source, reducing the risk of it spreading to your gut.
You should also consider how your diet affects both your gums and gut. Foods rich in fiber, probiotics, and nutrients—like leafy greens, yogurt, and whole grains—are great for both systems. Staying hydrated is equally important, as it helps maintain saliva flow to control oral bacteria.
Finally, managing systemic inflammation through lifestyle changes like regular exercise, stress management, and avoiding smoking can protect your overall health and reduce the risk of complications related to gum disease.
The Bottom Line
Your mouth and gut are more connected than you might think, and gum disease is a prime example of how oral health influences the rest of your body. By taking care of your gums, you’re also supporting a healthy gut—and vice versa. Addressing gum disease or digestive problems holistically can lead to better health from head to gut.

Healthy Gums Lead to a Healthy Gut
If you’re dealing with gum disease or digestive issues, it’s worth discussing these concerns with Dr. Scharf.